Слайд 2: Evaluation of New Attachment and Bone Regeneration
Clinical Methods Consist of: 1. Probing depth measurements (pre- and post-treatment). 2. Clinical gingival indices. 3. Determination of attachment level, care should be taken to measure the defect by placing the probe at the exact same point before and after treatment and also with the same angulation. Pre- and postoperative probing measurements without standardized method may not be reliable. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 3: Evaluation of New Attachment and Bone Regeneration
Radiographic Methods Standardized techniques for reproducible positioning of the film and tubing is very difficult. Even with standardization, the radiograph may not show the entire topography of the area before or after the treatment. Furthermore, thin bony trabeculae which was present before treatment may go undetected because minimal amount of mineralized tissue must be present to be seen or registered on the radiograph. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 4: Evaluation of New Attachment and Bone Regeneration
Surgical Re-entry This can give the best view of the state of the bone crest that can be compared with the one taken during the initial surgical intervention and can also be subjected to measurements. Even models can be used to appreciate the results of the therapy (pretreatment and post-treatment). This method is very useful but has two shortcomings: a. It requires a frequently unnecessary second operation. b. It does not show the type of attachment that exists (epithelial or connective tissue attachments). Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 5: Evaluation of New Attachment and Bone Regeneration
Histological Methods The type of attachment can only be determined by the histologic analysis of the tissue block taken from the healed area. Although this can give us the clear picture of regeneration of the attachment apparatus, it is not without problems. They are: a. The need to remove a tooth with its periodontium treated successfully limits the volunteers. b. Animal models (monkey, dog, pigs) can be used to clarify some aspects and but one must always remember the differences that exists when extrapolations to humans are attempted. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 6: The following reconstructive surgical techniques have been proposed
1. Nongraft -associated new attachment. 2. Graft-associated new attachment. 3. Combination of both. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 7: Nongraft -associated New Attachment
New attachment can be achieved without the use of grafts in : a. Meticulously treated three-walled defects ( Infrabony defect ). b. Perioendodontal abscesses. c. When the destructive procedure has occurred very rapidly, for example, after treatment of pockets which had acute periodontal abscess. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 8: Various techniques of nongraft -associated new attachment are :
Removal of Junctional and Pocket Epithelium Prevention of Epithelial Migration Guided Tissue Regeneration (GTR ) Clot Stabilization, Wound Protection and Space Creation Preparation of the Root Surface (Root Biomodification ) Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 9: Removal of Junctional and Pocket Epithelium
The methods used to do so include: i. Curettage — Only 50 percent of junctional epithelium and pocket epithelium can be removed. ii. Chemical agents — Mostly used in conjunction with curettage. The most commonly used drugs are sodium sulfide, phenol, camphor, sodium hypochlorite and antiformin. The main disadvantage is that the depth of action cannot be controlled. iii. Ultrasonic methods — It is again not very useful, because of lack of clinicians tactile sense while using these methods. iv. Surgical methods — • Excisional new attachment procedure with internal bevel incision (ENAP). • Gingivectomy procedure. • Modified Widman flap. • Coronal displacement of the flap. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 10: Prevention of Epithelial Migration
Eliminating junctional and pocket epithelium may not be sufficient because the epithelium from the excised margin may rapidly proliferate apically to become interposed between the healing connective tissue and cementum. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 11: Guided Tissue Regeneration (GTR)
This concept is based on the assumption that periodontal ligament cells have the potential for regeneration of the attachment apparatus of the tooth. Two types of membranes have been used: a. Degradable —Collagen, Polylactic acid, Vicryl and Guidor membrane. b. Nondegradable —They must be removed in three to six weeks time, e.g. Millipore, Teflon membrane, Goretex periodontal material. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
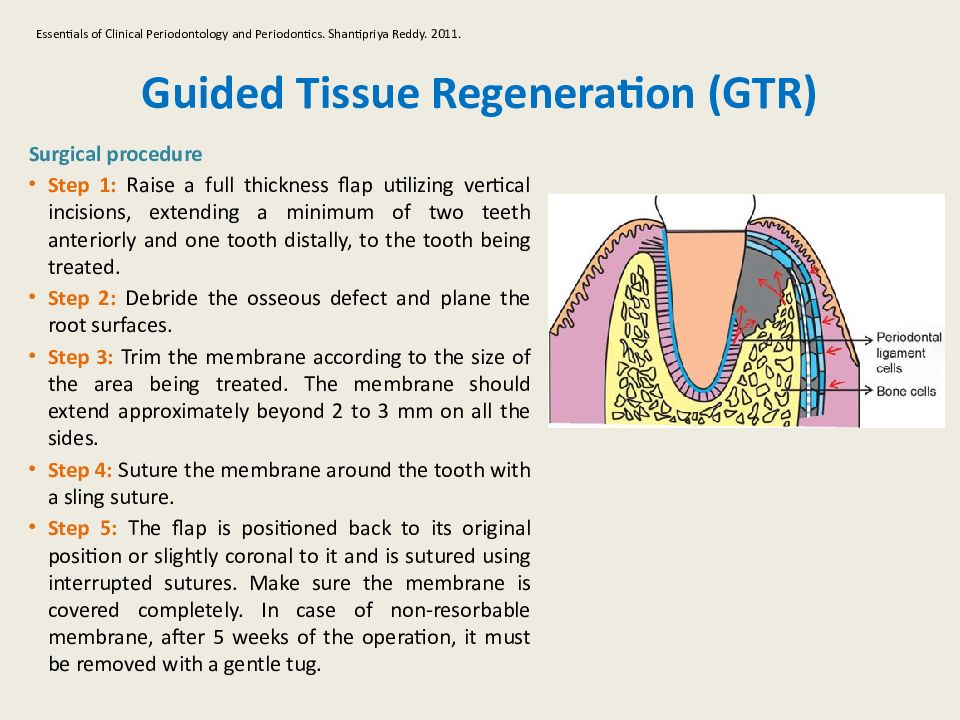
Слайд 12: Guided Tissue Regeneration (GTR)
Surgical procedure Step 1: Raise a full thickness flap utilizing vertical incisions, extending a minimum of two teeth anteriorly and one tooth distally, to the tooth being treated. Step 2: Debride the osseous defect and plane the root surfaces. Step 3: Trim the membrane according to the size of the area being treated. The membrane should extend approximately beyond 2 to 3 mm on all the sides. Step 4: Suture the membrane around the tooth with a sling suture. Step 5: The flap is positioned back to its original position or slightly coronal to it and is sutured using interrupted sutures. Make sure the membrane is covered completely. In case of non- resorbable membrane, after 5 weeks of the operation, it must be removed with a gentle tug. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 13: Clot Stabilization, Wound Protection and Space Creation
The successful results obtained with graft materials, barrier membranes and coronally -displaced flaps have been attributed to the fact that all of these protect the wound and create a space for undisturbed and stable maturation of the clot. Hence, this hypothesis suggests that preservation of the root surface that is, a fibrin clot interface prevents apical migration of the gingival epithelium and allows for connective tissue attachment during the early wound healing period. A lot of research is required to explore this possibility, for example, it requires more postoperative care, root conditioning to enhance fibrin clot and connective tissue attachment. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 14: Preparation of the Root Surface (Root Biomodification )
Several substances have been used to condition the root surface, for attachment of new connective, tissue fibers. These include citric acid, fibronectin and tetracycline. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 15: Preparation of the Root Surface (Root Biomodification )
Citric acid: When used with pH1 for two to three minutes on root surface, after surgical debridement, it produces surface demineralization, which inturn induces cementogenesis and attachment of collagen fibers. The following actions of citric acid have been reported by Register and Burdick in 1975. 1. It removes the smear layer and may open dentinal tubules, thus allowing cementum to form within these tubules creating the blunderbuss effect and produce cementum pins. This could be associated with accelerated cementogenesis. 2. It has also been shown to expose collagen fibers on the root surface, which may splice with the collagen fibers of a soft tissue graft or flap (called as collagen splicing) resulting in collagen adhesion without cementum formation and accelerated healing. 3. Epithelium does not migrate apically because of the accelerated healing either by connective tissue attachment or a collagen adhesion may occur before epithelium migrates. 4. Finally, citric acid, may demineralize small bits of residual calculus, disinfect the root surface and aid in removing endotoxins. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 16: Preparation of the Root Surface (Root Biomodification )
Steps involved: a. Raise full thickness flap. b. Perform thorough root planing. c. Apply cotton pellets soaked in citric acid pH1 for two to three minutes. d. Remove and irrigate root surface profusely with water. e. Replace the flap and suture. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 17: Preparation of the Root Surface (Root Biomodification )
Growth factors: They are polypeptide molecules released by the cells in the inflamed area, that regulates events in wound healing. These factors are primarily secreted by macrophages, endothelial cells, fibroblasts and platelets. They include platelet derived growth factor (PDGF), insulinlike growth factor (IGF), fibroblast growth factor (FGF) and TGF (transforming growth factor alpha and beta ). These can all be used to control events during periodontal wound healing, e.g. promoting proliferation of fibroblasts from periodontal ligament thereby favoring bone formation. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.
Слайд 18: Preparation of the Root Surface (Root Biomodification )
Enamel matrix proteins : This is based on the observations that amelogenin secreted by Hertwig’s epithelial root sheath during tooth development can induce acellular cementum formation which is believed to favor periodontal regeneration. Essentials of Clinical Periodontology and Periodontics. Shantipriya Reddy. 2011.